Jaison Jeevanandam, Senior Researcher, National Institute of Mental Health
Currently, our lab is working on an innovative convergence of nanomedicine and AI-based image processing to address neurodegenerative diseases. Nanoparticle carriers offer targeted brain delivery, while AI models analyse imaging data to optimise dosing and efficacy. In this interview, Dr. Jaison discusses about the promising, smarter, tailored interdisciplinary therapeutic strategies for conditions like Alzheimer’s and Parkinson’s disease.

1. How do you envision the convergence of nanomedicine and AI transforming the landscape of neurodegenerative disease therapy in the next decade?
Over the next decade, the fusion of nanomedicine and AI will redefine the treatment of neurodegenerative diseases, from merely managing symptoms to offering precision-modifying therapy. Smart nanocarriers will be engineered to traverse the blood–brain barrier, target specific brain cells and deliver controlled payloads, while AI leverages imaging and biomarker data (MRI, PET, molecular sensors) to optimise nanoparticle parameters like size, coating, ligand density, dose and release kinetics. The result will lead to faster, smarter, safer patient-specific, adaptive nanomedicine, ushering in a new era of precision neurotherapy.
2. What unique advantages do nanoparticle carriers provide in delivering therapeutics specifically to the brain, and how do they overcome the challenges of the blood-brain barrier?
Nanocarriers offer remarkable advantages for brain-targeted therapy by overcoming the blood–brain barrier (BBB). Their nanoscale size (10–200 nm) enables them to utilise natural BBB transport routes, like receptor- or adsorptive-mediated trans-cytosis via surface ligands such as transferrin or apolipoprotein mimetics. They safeguard therapeutics, provide controlled release, and can selectively target neurons, astrocytes, or microglia. In neurodegenerative diseases, where localised, sustained delivery is crucial, smart nanoparticles not only exploit but can also help repair BBB dysfunction, to offer a highly precise, efficient route for brain drug delivery.
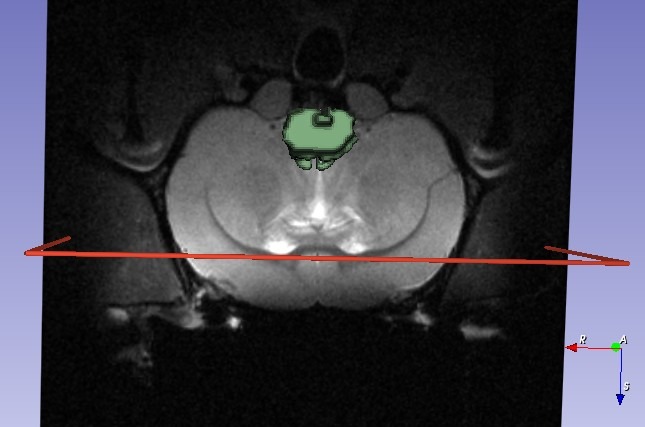
3. Could you elaborate on how AI-based image processing is enhancing the precision and efficacy of nanoparticle-mediated drug delivery?
AI-based image processing is rapidly becoming the backbone of next-generation nanoparticle drug delivery. It enhances precision by visualising nanoparticle biodistribution and uptake, feeding this data back into AI models to fine-tune particle design, dosage, and release patterns. According to me, AI and nanomedicine form an adaptive loop, where imaging, biomarkers, and predictive modeling guide personalised therapy. This synergy promises smarter, faster, and more effective treatments for neurodegenerative diseases, transforming how we design and deliver brain-targeted therapeutics.
AI-based imaging tools are transforming early detection in Alzheimer’s and Parkinson’s by identifying subtle brain changes like hippocampal atrophy, cortical thinning, or nigral degeneration that clinicians might overlook. Deep learning models using PET/MRI detect multimodal patterns, while diffusion MRI metrics reveal early micros.
4. In the context of diseases like Alzheimer’s and Parkinson’s, what specific biomarkers or imaging patterns are AI algorithms most effective in detecting?
Structural loss. Beyond brain scans, AI interprets retinal, voice, and gait biomarkers. I would say the real impact lies in converting complex imaging signatures into actionable, precision-guided biomarkers for enabling earlier diagnosis, better patient stratification, and real-time therapy monitoring.
5. How do AI models contribute to personalised dosing strategies in nanomedicine, and what data inputs are critical for their accuracy?
AI is redefining dosing in nanomedicine by connecting patient data, nanoparticle characteristics, and therapeutic outcomes. By analysing genetics, imaging, prior treatments, and nanoformulation details like size and coating, AI predicts how nanoparticles behave: how much reaches the target, how it releases drugs, and how the body clears it. Critical inputs include nanoparticle parameters, pharmacokinetic data, and patient physiology. Rather than replacing clinicians, AI enhances decision-making, helping design safer, optimised, and truly personalised dosing strategies for each patient.
6. What are the main ethical and safety considerations when combining AI-driven analysis with nanomedicine in clinical trials?
Combining AI with nanomedicine in clinical trials raises important safety and ethical questions. Nanoparticles may behave unpredictably, accumulating or causing immune reactions, so AI-driven dosing must not amplify these risks. Since AI often functions as a “black box,” transparency is key for informed consent. We must also address fairness, ensuring equal access and preventing healthcare disparities. Lastly, accountability is complex. When an AI-guided nanoparticle therapy fails, who’s responsible? I would say clear regulations and continuous safety monitoring are vital for responsible clinical integration.
7. How do you address interdisciplinary collaboration challenges between AI developers, nanotechnologists, and neuroscientists?
In interdisciplinary work between AI, nanotech, and neuroscience, the main challenge is aligning languages, timelines, and goals. We bridge gaps through shared vocabulary, frequent short meetings, and clear, measurable targets, like nanoparticle uptake or AI-predicted dosage. Cross-learning helps too; AI developers join lab demonstrations, and neuroscientists attend code reviews. This builds empathy and shared understanding. With flexible yet accountable leadership, any research team can shift from “three parallel groups” to one cohesive unit, which is essential for advancing AI-driven nanomedicine for brain disorders.
8. What are the major limitations or bottlenecks currently preventing widespread clinical adoption of AI-guided nanotherapeutics?
According to me, we are at an exciting crossroads where smart nanoparticles meet smart algorithms, but scaling AI-guided nanotherapeutics to clinics is not easy. The biggest hurdles are limited to patient-level datasets, difficulty replicating personalised nanoformulations, and costly, complex production with batch variability. Regulatory ambiguity, whether it is a drug, device, or digital therapy, also slows progress. Plus, what works in mice often fails in humans due to biological differences. The potential is huge, but solving these technical, regulatory, and translational bottlenecks is key to real-world adoption.
9. Can you discuss any successful preclinical or early clinical case studies where this combined approach has shown measurable efficacy?
While clinical trials of AI-guided nanotherapeutics in neurodegeneration are limited, preclinical studies show promise. For example, BBB-penetrating nanoparticles delivering BACE1 gene-silencing agents in Alzheimer’s mice reduced amyloid plaques and improved cognition. In Parkinson’s models, focused ultrasound combined with GDNF-loaded nanoparticles achieved widespread brain delivery and behavioural recovery. These studies highlight precise, targeted delivery and measurable outcomes. Integrating imaging and AI-driven feedback loops into such platforms will further optimise dosage and formulation, paving the way toward translational, patient-specific nanomedicine therapies.
10. How does AI facilitate real-time monitoring of therapeutic outcomes and patient response in neurodegenerative conditions?
I would say AI is transforming real-time monitoring in neurodegenerative therapy by analysing imaging, sensor, and longitudinal data to track patient response. It detects subtle changes in retinal scans, MRI, PET, or physiological signals, showing whether nanoparticle treatments reach targets and have effects. Adaptive, closed-loop systems can flag plateaus or drops in biomarker changes, guiding clinicians to adjust doses or timing. By combining AI’s analytical power with nanomedicine’s precision delivery, we can personalise therapy, monitor outcomes continuously, and respond faster than traditional methods.
11. In your opinion, what role will predictive modeling and simulation play in designing next-generation nanomedicine interventions?
Predictive modeling and simulation are revolutionising nanomedicine design, especially for brain targets. They let us virtually test nanoparticle properties, such as size, shape, coatings, ligands, and predict circulation, BBB crossing, cellular interactions, and clearance, reducing trial-and-error experiments. Coupled with AI, these models integrate patient-specific data like imaging, genomics, and disease stage to suggest optimal nanoparticle design and dosing. They also inform smarter clinical pathways, accelerating translation while minimising risk. Essentially, simulations act as the blueprint, guiding safe, personalised, and effective nanomedicine development.
12. How can regulatory frameworks keep pace with the rapid evolution of AI-nanomedicine convergence while ensuring patient safety?
Combining AI with nanomedicine demands forward-thinking regulation. Adaptive frameworks are key, allowing continuous monitoring, re-certification, and real-world evidence feedback as AI models and nanoparticle designs evolve. A risk-based approach is also essential, assessing the hybrid nature of drug-device-software therapies. Regulators must evaluate nanoparticle materials, AI algorithm integrity, and clinical context together. In my opinion, emerging frameworks, like the EU’s AI Act and Medical Device Regulation, can illustrate how overlapping, flexible policies can safeguard patient safety while keeping pace with rapid innovation.
13. What are the potential risks of over-reliance on AI in therapeutic decision-making, and how can clinicians maintain a human-centric approach?
In my view, over-reliance on AI in therapeutic decisions carries real risks. While AI can analyse vast data and suggest therapies, it may miss patient-specific context, such as lifestyle, values and subtle clinical cues. Limited or biased datasets can lead to inaccurate recommendations, amplifying health inequities. Clinicians who treat AI outputs as gospel risk safety and ethical issues, and may even see their own diagnostic skills erode. Maintaining a human-centric approach means using AI as a tool, not a replacement, while critically evaluating its suggestions.
14. Looking ahead, what emerging technologies or innovations could further enhance the synergy between AI and nanomedicine for brain disorders?
Looking ahead, emerging technologies like cell-membrane-engineered nanoparticles, embedded sensors, and neuromorphic AI could dramatically enhance AI-nanomedicine synergy for brain disorders. These nanoparticles can evade the immune system, cross the BBB efficiently, and deliver personalised payloads, while AI optimises ligand design and cargo based on patient-specific profiles. Real-time feedback from sensors can adjust dosing dynamically, and generative AI models can predict and prioritise nanoparticle formulations, reducing trial-and-error experiments and enabling smarter, responsive, region-specific therapies for neurodegeneration.
‘’The future is not just about tiny particles or big data. It is about dynamic systems where nano-engineering, realistic models and AI decision-layers all talk to each other.’’
If you are working on brain disorder treatment, where the barriers are huge and the stakes are high, these innovations are not optional, they are essential.
References
- Jeevanandam, J., Tsenov, G., Danquah, M.K., Ruiz-Molena, D., Boussios, S. and Ovsepian, S.V., 2025. Smart Nanomedicines for Neurodegenerative Diseases: Empowering New Therapies with Molecular Imaging and Artificial Intelligence: J. Jeevanandam et al. Molecular Diagnosis & Therapy, pp.1-28.
- Roney, C., Kulkarni, P., Arora, V., Antich, P., Bonte, F., Wu, A., Mallikarjuana, N.N., Manohar, S., Liang, H.F., Kulkarni, A.R. and Sung, H.W., 2005. Targeted nanoparticles for drug delivery through the blood–brain barrier for Alzheimer’s disease. Journal of controlled release, 108(2-3), pp.193-214.
- Liu, J., Wang, T., Dong, J. and Lu, Y., 2025. The blood–brain barriers: novel nanocarriers for central nervous system diseases. Journal of Nanobiotechnology, 23(1), p.146.
- Mehdizadeh, S., Mamaghani, M., Hassanikia, S., Pilehvar, Y. and Ertas, Y.N., 2025. Exosome-powered neuropharmaceutics: unlocking the blood-brain barrier for next-gen therapies. Journal of Nanobiotechnology, 23(1), p.329.
- Gao, L., Wang, J. and Bi, Y., 2025. Nanotechnology for Neurodegenerative Diseases: Recent Progress in Brain-Targeted Delivery, Stimuli-Responsive Platforms, and Organelle-Specific Therapeutics. International Journal of Nanomedicine, pp.11015-11044.
- Liu, J., Wang, T., Dong, J. and Lu, Y., 2025. The blood–brain barriers: novel nanocarriers for central nervous system diseases. Journal of Nanobiotechnology, 23(1), p.146.
- Chow, J.C., 2025. Nanomaterial-based molecular imaging in cancer: advances in simulation and AI integration. Biomolecules, 15(3), p.444.
- Tomitaka, A., Vashist, A., Kolishetti, N. and Nair, M., 2023. Machine learning assisted-nanomedicine using magnetic nanoparticles for central nervous system diseases. Nanoscale Advances, 5(17), pp.4354-4367.
- He, S., Abarrategi, J.S., Bediaga, H., Arrasate, S. and González-Díaz, H., 2024. On the additive artificial intelligence-based discovery of nanoparticle neurodegenerative disease drug delivery systems. Beilstein Journal of Nanotechnology, 15(1), pp.535-555.
- Khorsandi, D., Farahani, A., Zarepour, A., Khosravi, A., Iravani, S. and Zarrabi, A., 2025. Bridging technology and medicine: artificial intelligence in targeted anticancer drug delivery. RSC advances, 15(34), pp.27795-27815.
- Chang, Y., Liu, J., Sun, S., Chen, T. and Wang, R., 2025. Deep learning for Parkinson’s disease classification using multimodal and multi-sequences PET/MR images. EJNMMI research, 15(1), p.55.
- Kumar, R.; Waisberg, E.; Ong, J.; Paladugu, P.; Amiri, D.; Saintyl, J.; Yelamanchi, J.; Nahouraii, R.; Jagadeesan, R.; Tavakkoli, A. Artificial Intelligence-Based Methodologies for Early Diagnostic Precision and Personalized Therapeutic Strategies in Neuro-Ophthalmic and Neurodegenerative Pathologies. Brain Sci. 2024, 14, 1266.
- Nikparast, F., Ganji, Z. and Zare, H., 2022. Early differentiation of neurodegenerative diseases using the novel QSM technique: what is the biomarker of each disorder?. BMC neuroscience, 23(1), p.48.
- Tukur, H.N., Uwishema, O., Akbay, H., Sheikhah, D. and Correia, I.F.S., 2025. AI-assisted ophthalmic imaging for early detection of neurodegenerative diseases. International Journal of Emergency Medicine, 18(1), p.90.
- Mazumdar, H., Khondakar, K.R., Das, S., Halder, A. and Kaushik, A., 2025. Artificial intelligence for personalized nanomedicine; from material selection to patient outcomes. Expert Opinion on Drug Delivery, 22(1), pp.85-108; Bae, H., Ji, H., Konstantinov, K., Sluyter, R., Ariga, K., Kim, Y.H. and Kim, J.H., 2025. Artificial Intelligence‐Driven Nanoarchitectonics for Smart Targeted Drug Delivery. Advanced Materials, p.e10239; Vora, L.K., Gholap, A.D., Jetha, K., Thakur, R.R.S., Solanki, H.K. and Chavda, V.P., 2023. Artificial intelligence in pharmaceutical technology and drug delivery design. Pharmaceutics, 15(7), p.1916.
- Hassan, Y.M., Wanas, A., Ali, A.A. and El-Sayed, W.M., 2025. Integrating artificial intelligence with nanodiagnostics for early detection and precision management of neurodegenerative diseases. Journal of Nanobiotechnology, 23(1), p.668.
- Youssef, A., Nichol, A.A., Martinez-Martin, N., Larson, D.B., Abramoff, M., Wolf, R.M. and Char, D., 2024. Ethical considerations in the design and conduct of clinical trials of artificial intelligence. JAMA network open, 7(9), pp.e2432482-e2432482.
- Wang, K., Yang, R., Li, J., Wang, H., Wan, L. and He, J., 2025. Nanocarrier-based targeted drug delivery for Alzheimer’s disease: addressing neuroinflammation and enhancing clinical translation. Frontiers in Pharmacology, 16, p.1591438.
- Duan, L., Li, X., Ji, R., Hao, Z., Kong, M., Wen, X., Guan, F. and Ma, S., 2023. Nanoparticle-based drug delivery systems: an inspiring therapeutic strategy for neurodegenerative diseases. Polymers, 15(9), p.2196.
- Contreras, L.F.H., Truong, N.D., Eshraghian, J.K., Xu, Z., Huang, Z., Nikpour, A. and Kavehei, O., 2023. Neuromorphic neuromodulation: Towards the next generation of on-device AI-revolution in electroceuticals. arXiv preprint arXiv:2307.12471.
Author Bio

Dr. Jaison Jeevanandam is a researcher in the Division of Experimental Neurobiology, Preclinical Research Program, at the National Institute of Mental Health (Czechia). His work integrates nanomedicine, molecular imaging, and artificial intelligence to develop next-generation treatments for neurological disorders. He leads initiatives to translate technologies from bench to bedside through international collaborations across Europe, Asia, and the United States.




