Schizophrenia Diagnosis and Social Impacts
The diagnosis of schizophrenia is usually based only on observing behavior, while the origin of the illness remains unclear. That is why immunologist Ivana Kawiková considers it crucial to study these disorders in the broader context of the overall development of the organism, even before the disease itself manifests. Thanks to the support of the MERIT program, she works at the National Institute of Mental Health. What are the possibilities for the future treatment of schizophrenia? And how can we move from research to practice? You will learn not only that in our interview.
According to WHO surveys, about 24 million people worldwide suffer from schizophrenia. What is the situation in the Czech Republic?
In the Czech Republic, it is estimated that about 100,000 people suffer from schizophrenia. But it is important to stress that schizophrenia is not a single disease in the strict sense, but rather a syndrome – a set of symptoms that may be caused by different biological disorders. So far, however, we have no objective diagnostic tests to distinguish between these biological pathways. Once we are able to do that, we will also have tools to better select medications.
From clinical practice, we know that the impact of the disease goes far beyond the individual – it strongly affects their immediate surroundings as well. Patients with schizophrenia have a much higher risk of suicide, and their families or friends often suffer from what is happening to their loved ones. Especially in the Czech Republic, where there is still a lack of a quality network of follow-up care and community services, the situation is very demanding for both patients and their surroundings.

But you are not a psychiatrist. Your professional career is strongly interdisciplinary, and you also finished school in the breakthrough post-revolutionary period. How did you get abroad back then?
During my pediatrics studies at Charles University, an essential encounter for me was with Jan Herget, who directed me toward pathophysiology and involved me in my first research projects in this area. After completing my medical studies, I taught pathophysiology, which gave me a strong foundation not only in expertise but also in pedagogy – I learned how to communicate with students about what happens when one of the body’s systems fails to function properly.
After 1989, new opportunities appeared. In 1991 I received a two-year fellowship from the Swedish Lung and Heart Foundation for a stay at the University of Gothenburg. I was thrilled, but leaving was not easy. It was shortly after the Velvet Revolution, the atmosphere here was full of hope, and I knew I would miss home a lot. I decided to try for three months and then see. I worked in pharmacology and physiology of inflammatory mediators in the airways and skin under the supervision of Jan Lotvall. In the end, I also received a fellowship for my entire doctoral studies, which opened up the opportunity to complete part of my Ph.D. project at Imperial College London under Sir Peter Barnes and Maria Belvisi.
And how did you move from pathophysiology, pharmacology, and immunology to psychology and psychiatry?
I focused on experimental and clinical immunology especially during my postdoctoral fellowship at Yale University School of Medicine under Philip Askenase. After postdoctoral training, I began working as an independent researcher. At that time, a key impulse came from James F. Leckman, now Professor Emeritus of Child Psychiatry at Yale, who approached me with research focused on the hypothesis that Tourette’s syndrome, whose prominent symptom is tics, might have an autoimmune basis.
I had a friend who, during medical school, contracted infectious mononucleosis caused by the EBV virus, which scientists suspect may be a factor in many other diseases. After this illness, my friend completely changed. A calm and cheerful person began to suffer from severe anxiety and later schizophrenia, which for a long time did not respond to any medication. I observed this for a long time and knew that even the best doctors here could not help him.
So I could not refuse James Leckman’s proposal to study the autoimmune nature of other mental disorders, and I never regretted it. Working with him was excellent, and we proved that in a subgroup of children with Tourette’s syndrome, the immune system plays an important role. Later, it turned out this is also the case for other psychiatric disorders.
Diagnostic Markers of Mental Disorders
What are the biggest limits of current treatment in the field of mental disorders, especially schizophrenia, which your research focuses on?
The main problem is that these diseases still lack objective diagnostic biomarkers – we mostly rely only on behavioral observations, and the origin of the illness remains unclear. We could learn a lot from intervention studies, where we actively influence the course of care and the patient’s life, but this is problematic with immunological pathway blockade, as we do not want to reduce the patient’s defense against microorganisms. That is why I consider it key to study these disorders in the broader context of the organism’s development, even before the disease itself manifests. In this respect, I value my previous experiences in the above-mentioned areas of medicine.
Have you managed within the MERIT program to advance markers of mental illness? For example, in schizophrenia, which is often accompanied by psychosis?
I would like to highlight the ESO (Early Schizophrenia Outcome) project, within which the world’s largest database of patients with First Episode Psychosis (FEP) was created. The project is led by my colleague and MERIT mentor Filip Španiel, head of the Center for the Research of First Episodes of Severe Mental Illness (SMI) at the National Institute of Mental Health. The study combines MRI data with long-term clinical monitoring of patients and the pathophysiological processes in their bodies.
It is crucial that MRI scans are taken at the onset of the illness, then again after one year, and after two years. Filip Španiel found that the most significant morphological changes in the brain occur during the first year of the illness. Based on these changes, patients were divided into three groups according to cortical development: thickened cortex, thinned cortex, and a group without apparent changes.

How does your research build on this?
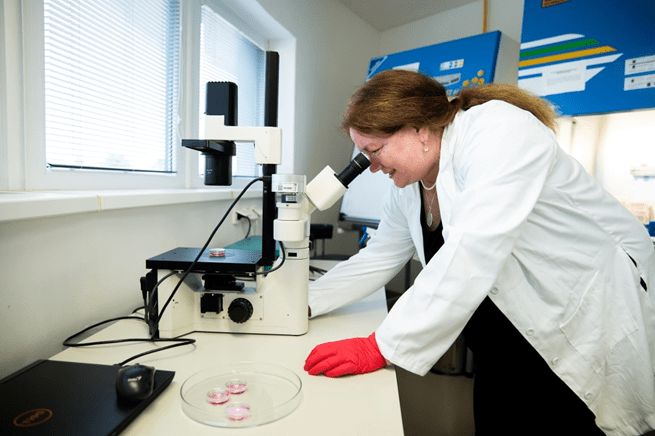
Our follow-up research directly builds on these findings. We focus on the analysis of patients’ blood samples to examine whether biomarkers distinguishing these groups can be identified at an early stage of the illness. If confirmed, we could create a diagnostic panel enabling individualized treatment right at the onset of the illness.
In this context, it is also important to mention current therapeutic options. For example, Clozapine is used in schizophrenia only as a last-resort treatment, when other antipsychotics fail. But in some patients, this drug can be associated with severe side effects – it can negatively affect bone marrow function, leading to suppression of white blood cell production. The consequence is an increased risk of infections and immunodeficiency, which poses a clinical risk. Some researchers believe this drug may prevent degenerative brain changes in the early stages of schizophrenia. If proven, Clozapine might begin to be administered at the start of the illness, perhaps only temporarily, with more intensive monitoring of immune functions than today and with readiness to address possible immunodeficiency immediately.
Not only this approach, but also other potential procedures could lead to more personalized and effective treatment already in the early stages of the illness.
Do the outcomes of your research have the potential to go beyond schizophrenia treatment? Could they be applied to other psychiatric disorders as well?
That is indeed our hope. The principle of our research – longitudinal monitoring of a large number of patients combined with advanced imaging methods and pioneering experimental analyses of blood and stool samples – has strong potential to bring new know-how also for diagnosing and treating other psychiatric disorders.
At NIMH you initiated a new educational format for scientists – the Journal Club, a discussion of new publications in high-impact journals. What inspired you to introduce it, and what activities take place within it?
The inspiration was my postdoctoral fellowship at Yale School of Medicine, where a similar format was led by Philip W. Askenase, head of the Allergy & Clinical Immunology section. The Journal Club was held every Wednesday and offered participants pizza and an excellent opportunity to present an article from a prestigious journal of their choice and interest.
The beauty of this format was that it did not matter whether the presenter was an expert in the field or a beginning student – what mattered was the quality and precision of preparation. Thanks to these meetings, I gradually gained a fairly broad and comprehensive overview across various areas of biomedicine.
I later adopted this concept in my further teaching activities, and it proved very effective. After returning to the Czech Republic, I noticed a certain lack of scientific interaction, even though students clearly crave such activities. Although organizing the Journal Club is time-consuming and sometimes even exhausting and “painful” (laughs), I believe this investment pays off in the form of higher-quality education. We successfully completed the first semester, and I am convinced this format has real value.
Flexibility of the MERIT Program
How did you actually get into the MERIT program?
I had considered returning to the Czech Republic earlier. My colleague Karel Valeš from NIMH first invited me for a three-month stay within the Mobility Fellowship. He also told me about the MERIT program. While reading the conditions of the program, I realized it was a great opportunity. I would especially like to highlight the freedom and flexibility the program provides. I also value the fact that as part of the fellowship it includes support for networking with experts, for example by attending conferences.
The MERIT program also requires participation at two other institutions (so-called secondment places), one of which must be abroad. How is cooperation with these institutions going?
For the foreign institution, I relied on my previous experience and therefore chose the Yale School of Medicine, where I had already worked. Thanks to my knowledge of the environment and existing contacts, I can smoothly continue previous work, which greatly facilitates research activities within the MERIT program.
The second institution is the Czech biotechnology company Essence Line, which focuses on research, development, and laboratory services in biochemical analysis. Collaboration with Petr Novotný is very intensive, both in the context of potential future commercialization of research results and in the practical organization of measurements. At this workplace, we currently focus on the analysis of inflammatory molecules and biomarkers released from the brain and subsequently circulating freely in the body, or conversely, present in the blood for other reasons and affecting the brain.
What do you especially appreciate about the MERIT program?
I consider the overall combination of flexibility and emphasis on the practical use of research to be very well designed. I would be glad if there were more opportunities like this. You may be surprised that I also view positively the system of ongoing monitoring through semi-annual progress reports. Feedback from the Central Bohemian Innovation Center (SIC) is effective and has opened up further opportunities, such as consultations on spin-offs, which I am only beginning to learn about.
As a researcher, I am used to “only” designing a project, implementing it, and publishing results in a scientific journal. The area of commercialization is new to me. I appreciate that the MERIT program also provides significant support in this regard – whether in the form of workshops or direct connections with experts specializing in research commercialization.
Ivana Kawiková is a fellow of the MERIT program at the National Institute of Mental Health (NIMH), where she researches markers of mental disorders using schizophrenia as an example. In the past, she worked in Sweden, England, and the USA on eicosanoids and on both traditional and humanized models of inflammatory diseases, as well as on the role of inflammatory processes in developmental disorders such as autism and Tourette’s syndrome.